髋臼周围截骨术随访30年,临床效果究竟如何?
2018-07-04 文章来源:304关节学术 作者:译者:张振东 编辑:骨科在线 点击量:2738 我要说
由TD Lerch、SD Steppacher等人发表于《Clin Orthop Relat Res》杂志的一项对髋臼周围截骨术(periacetabular osteotomy,PAO)后30年随访的研究显示,早期PAO术后30年,29%的髋关节达到成功保髋,但超过70%的患者会发生骨关节炎进展、髋关节疼痛和/或接受THA。
PAO自从1984年首次提出以来,已被广泛用于治疗髋关节发育不良(DDH)。但对其术后30年的保髋生存率尚无报道。由于PAO治疗的患者往往比较年轻,长期随访并明确预后因素有助于合理选择手术适应证。因此研究人员通过对最初接受PAO治疗的患者随访,以明确:(1)以下研究终点事件的30年累积生存率:接受关节置换术(THA)、骨关节炎进展、Merle d'Aubigné-Postel评分 < 15;(2)髋关节功能及疼痛是否改善;(3)骨关节炎是否进展;(4)与3个研究终点事件相关的因素。
研究人员回顾性分析了1984年至1987年接受PAO治疗的63例(75髋)DDH患者。最初DDH为PAO的唯一适应证,因此研究仅包括DDH患者而不包括因髋臼后倾接受PAO的患者。术前骨关节炎2期及以上者18髋(24%),既往股骨和/或髋臼有手术史者22例(23髋[31%])。截止末次随访,39例(42髋[56%])接受关节置换治疗,1例(1髋[1%])接受髋关节融合术治疗。2例患者分别在术后6年、16年因其他非手术相关因素死亡。其他21例(29髋)平均随访时间为29年(范围:27-32年),其中5例(6髋[8%])最近未随访而仅有1次随访表可用。根据K-M生存分析,计算以下3个终点事件发生的累积生存率:接受关节置换术(THA)、骨关节炎进展、Merle d'Aubigné-Postel评分 < 15。使用Merled'Aubigné-Postel评分、髋关节Harris评分、步态及髋关节前后撞击试验评估髋关节疼痛及功能情况。使用Tönnis骨关节炎分期评估骨关节炎进展情况。Cox回归模型用来明确与以上3个研究终点事件相关的因素。
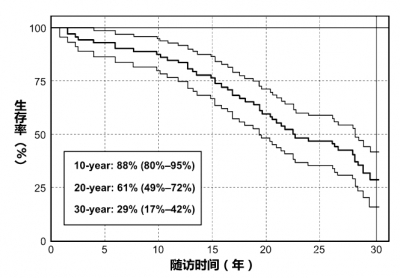
图1 PAO术后随访30年生存率情况。终点事件:接受关节置换术(THA)、骨关节炎进展、Merle d'Aubigné-Postel评分<15
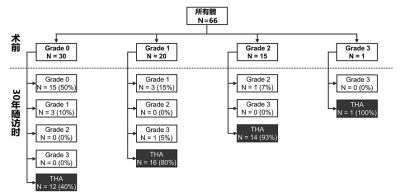
图2 术前与随访30年Tönnis骨关节炎分期评估
结果显示,PAO术后未发生3个研究终点事件的30年累积生存率为 29% (95%CI, 17%-42%)。Merle d'Aubigné-Postel评分 (15 ± 2 vs. 16 ± 2,p = 0.144) 及髋关节Harris评分 (83 ± 11 vs. 85 ± 17, p = 0.602)均未改善。髋关节前撞击试验(+)患者的比例降低(39% vs. 14%, p = 0.005),而髋关节后撞击试验(+)患者的比例并没有降低(14% vs. 3%, p = 0.592)。跛行的患者比例由术前66%降至30年随访时的18%(p < 0.001)。骨关节炎分期由术前0.8 ± 1 (0-3)进展至 2.1 ± 1(0-3)。10个因素与3个终点事件发生相关:手术年龄大于40岁 (风险比[HR] 4.3[3.7-4.9]);术前Merle d'Aubigné-Postel评分 < 15 (HR 4.1 [3.5-4.6]);术前髋关节Harris评分< 70 (HR 5.8 [5.2-6.4]);术前跛行 (HR 1.7 [1.4-1.9]);术前前撞击(+) (HR 3.6 [3.1-4.2]);术前后撞击(+) (HR 2.5 [1.7-3.2]);术前内旋 < 20° (HR 4.3 [3.7-4.9]);术前Tönnis骨关节炎分期 > 1 (HR 5.7 [5.0-6.4]);术后前覆盖 > 27%(HR 3.2 [2.5-3.9]);术后髋臼后倾 (HR 4.8 [3.4-6.3])。
作者表示,PAO可有效治疗有症状的DDH患者,但对于术前骨关节炎分期≥ 2的患者,不应行PAO治疗。术后髋臼过度覆盖或术后髋臼后倾与术后关节生存率的降低有关。
原文摘要:
One-thirdof Hips After Periacetabular Osteotomy Survive 30 Years With Good ClinicalResults, No Progression of Arthritis, or Conversion to THA
BACKGROUND: Since itsfirst description in 1984, periacetabular osteotomy (PAO) has become anaccepted treatment for hip dysplasia. The 30-year survivorship with thisprocedure has not been reported. Because these patients are often very young atthe time of surgery, long-term followup and identification of factors associatedwith poor outcome could help to improve patient selection.
QUESTIONS/PURPOSES: Looking atthe initial group of patients with hip dysplasia undergoing PAO at theoriginator's institution, we asked: (1) What is the cumulative 30-year survivalrate free from conversion to THA, radiographic progression of osteoarthritis,and/or a Merle d'Aubigné-Postel score < 15? (2) Did hip function improve andpain decrease? (3) Did radiographic osteoarthritis progress? (4) What are thefactors associated with one or more of the three endpoints: THA, radiographicprogression of osteoarthritis, and/or Merle d'Aubigné-Postel score < 15?
METHODS: Weretrospectively evaluated the first 63 patients (75 hips) who underwent PAO forhip dysplasia between 1984 and 1987. At that time, hip dysplasia was the onlyindication for PAO and no patients with acetabular retroversion, the secondindication for a PAO performed today, were included. During that period, noother surgical treatment for hip dysplasia in patients with closed triradiatecartilage was performed. Advanced osteoarthritis (≥Grade 2 according to Tönnis) was present preoperatively in 18 hips (24%) and 22patients (23 hips [31%]) had previous femoral and/or acetabular surgery.Thirty-nine patients (42 hips [56%]) were converted to a THA and one patient(one hip [1%]) had hip fusion at latest followup. Two patients (three hips[4%]) died from a cause unrelated to surgery 6 and 16 years after surgery withan uneventful followup. From the remaining 21 patients (29 hips), the meanfollowup was 29 years (range, 27-32 years). Of those, five patients (six hips[8%]) did not return for the most recent followup and only a questionnaire wasavailable. The cumulative survivorship of the hip according to Kaplan-Meier wascalculated if any of the three endpoints, including conversion to THA,progression of osteoarthritis by at least one grade according to Tönnis, and/ora Merle d'Aubigné-Postel score < 15, occurred. Hip pain and function wereassessed with Merle d'Aubigné-Postel score, Harris hip score, limp, andanterior and posterior impingement tests. Progression of radiographicosteoarthritis was assessed with Tönnis grades. A Cox regression model was usedto calculate factors associated with the previously defined endpoints.
RESULTS: Thecumulative survivorship free from conversion to THA, radiographic progressionof osteoarthritis, and/or Merle d'Aubigné-Postel score < 15 was 29% (95%confidence interval, 17%-42%) at 30 years. No improvement was found for eitherthe Merle d'Aubigné-Postel (15 ± 2 versus 16 ± 2, p = 0.144) or Harris hipscore (83 ± 11 versus 85 ± 17, p = 0.602). The percentage of a positiveanterior impingement test (39% versus 14%, p = 0.005) decreased at 30-yearfollowup, whereas the percentage of a positive posterior impingement test (14%versus 3%, p = 0.592) did not decrease. The percentage of positive limpdecreased from preoperatively 66% to 18% at 30-year followup (p < 0.001).Mean osteoarthritis grade (Tönnis) increased from preoperatively 0.8 ± 1 (0-3) to2.1 ± 1 (0-3) at 30-year followup (p < 0.001). Ten factors associated withpoor outcome defined as THA, radiographic progression of osteoarthritis, and/orMerle d'Aubigné-Postel score < 15 were found: preoperative age > 40 years(hazard ratio [HR] 4.3 [3.7-4.9]), a preoperative Merle d'Aubigné-Postel score< 15 (HR 4.1 [3.5-4.6]), a preoperative Harris hip score < 70 (HR 5.8[5.2-6.4]), preoperative limp (HR 1.7 [1.4-1.9]), presence of a preoperativepositive anterior impingement test (HR 3.6 [3.1-4.2]), presence of apreoperative positive posterior impingement test (HR 2.5 [1.7-3.2]), apreoperative internal rotation of < 20° (HR 4.3 [3.7-4.9]), a preoperativeTönnis Grade > 1 (HR 5.7 [5.0-6.4]), a postoperative anterior coverage >27% (HR 3.2 [2.5-3.9]), and a postoperative acetabular retroversion (HR 4.8[3.4-6.3]).
CONCLUSIONS: Thirtyyears postoperatively, 29% of hips undergoing PAO for hip dysplasia can bepreserved, but more than 70% will develop progressive osteoarthritis, pain,and/or undergo THA. Periacetabular osteotomy is an effective technique to treatsymptomatic hip dysplasia in selected and young patients with closed triradiatecartilage. Hips with advanced joint degeneration (osteoarthritis Tönnis Grade ≥ 2)should not be treated with PAO. Postoperative anterior acetabular overcoverageor postoperative acetabular retroversion were associated with decreased jointsurvival.
文献出处:Lerch TD,Steppacher SD, Liechti EF, Tannast M, Siebenrock KA. One-third of Hips AfterPeriacetabular Osteotomy Survive 30 Years With Good Clinical Results, NoProgression of Arthritis, or Conversion to THA. Clin Orthop Relat Res. 2017Apr;475(4):1154-1168.



 京公网安备11010502051256号
京公网安备11010502051256号