旋转中心间距:预测DDH患者OA进展的影像学新参数
2019-02-13 文章来源:骨科在线 点击量:1501 我要说
来源:304关节学术
译者:罗殿中
整理:骨科在线
由Morita D等人发表于《Clin Orthop Relat Res》杂志的一项研究显示,股骨头旋转中心较髋臼旋转中心在水平方向的移位记录距离,与髋关节发育不良(DDH)患者骨关节炎进展间存在轻度的相关性。
畸形程度相仿的DDH患者骨关节炎(OA)进展速度可能存在差异。尽管头臼匹配程度可能与骨关节炎的进展相关,但这是一种主观的判定。对于双侧DDH患者,接受保髋治疗患者的对侧髋关节OA进展或疼痛情况进展的概率有多大?旋转中心间距与OA进展或症状进展间是否存在关联?旋转中心间距与其它影像学参数间是否存在关联?因此研究者试图测量髋臼旋转中心与股骨头旋转中心间的距离,并分析其与DDH患者OA进展间的关系。
作者纳入了自1989年7月至1999年12月,在其所在中心接受偏心髋臼旋转截骨术治疗,共297名(319髋)患者。在这个时间段就诊的DDH患者,没有接受其它方式的保髋手术治疗。纳入标准包括:年龄小于55岁,对侧关节Tönnis骨关节炎分期0期,没有既往髋关节手术史,手术时对侧关节无症状。满足上述要求的共有155名(155髋)患者。排除保准包括:单侧DDH(4名患者,4髋),随访少于10年(42名,42髋),病历或影像学资料丢失(21名,21髋)。剩余88名(88髋)患者平均年龄39岁(17-53岁),11男77女,术后平均随访20年(10-27年)。在患者骨盆正位X线片上测量各影像学参数,明确患者术后1年及以后随访的Tönnis骨关节炎分期。研究人员将股骨头旋转中心较髋臼旋转中心在水平方向的移位记录为X距离(mm),在垂直方向的移位记录为Y距离(mm),同时测量两个旋转中心间的直线距离。通过进行K检验得出组内及组间一致性分别为:0.896,0.857(X距离);0.912,0.874(Y距离);0.912,0.901(直线距离)。当患者感觉对侧关节出现任何疼痛时,即判定为症状出现。通过Kaplan-Meier分析描述非手术侧关节骨关节炎进展及症状出现情况。使用Cox比例风险模型进行多变量分析以评估每个结果的风险因子。应用相关分析明确旋转中心间距与其它影像学参数(外侧CE角、股骨头非覆盖率、髋臼深度宽度指数、股骨头外移距离、关节间隙最小距离、股骨头圆度、头臼匹配度)间的关系,计算Pearson's相关系数。
结果显示,术后20年随访显示非手术侧髋关节骨关节炎进展的比例为13%(95%置信区间[CI],7.1-22.1),进展出现症状的比例为34%(95% CI,24.7-46.1)。各组X距离分别为:骨关节炎组(外移2.0± 2.1mm)、非骨关节炎组(内移0.4 ± 2.1 mm);症状进展组(外移0.9 ± 2.4 mm)、非症状进展组(内移0.5 ± 2.0 mm),两组间差异均有统计学意义(p < 0.001;p = 0.005)。各组Y距离分别为:骨关节炎组(下移2.7 ± 7.1 mm)、非骨关节炎组(上移1.6 ± 6.2 mm);症状进展组(下移2.1 ± 6.0 mm)、非症状进展组(上移2.5 ± 6.1 mm),两组间差异均有统计学意义(p = 0.027;p = 0.001)。导致骨关节炎进展的危险因素包括股骨头非覆盖率(危险比1.11;95% CI, 1.01-1.22; p = 0.028)、X距离(危险比1.52; 95% CI, 1.07-2.16; p = 0.019)。尚未发现导致症状出现的危险因素。X距离与其它影像学参数间无相关性。
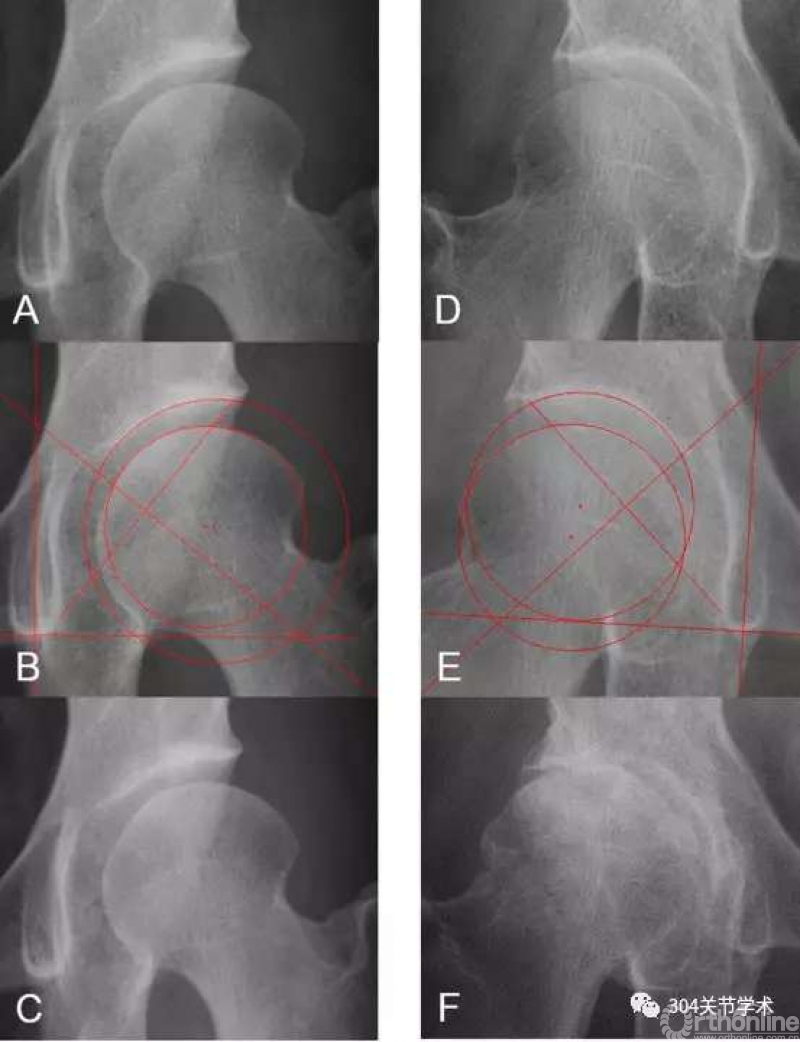
A:34岁女性DDH患者,非手术侧外侧CE角13°;B:X距离为内移2mm;C:22年后关节仍无骨关节炎进展;
D:43岁女性DDH患者,非手术侧外侧CE角23°;E:X距离为外移1.8mm;F:18年后骨关节炎进展
作者表示,未来需要对没有DDH患者的旋转中心间距进行测量,计算正常值,同时还需要在侧位片测量旋转中心间距。
原文摘要:
A Possible New Radiographic Predictor of Progression ofOsteoarthritis in DevelopmentalDysplasia of the Hip: The Center Gap
BACKGROUND:
Patients with comparableseverities of developmental dysplasia of the hip (DDH) may variably progress toosteoarthritis (OA) over time. Although joint congruency may be associated withOA progression in patients with DDH, it has only been assessed subjectively. Weassessed the gap between the rotational centers of the acetabulum and femoralhead (center gap) as a possible predictive measure of OA progression inpatients with DDH.
QUESTIONS/PURPOSES:
In patients with bilateralDDH, we asked: (1) What is the probability of OA progression (Tönnis grade) orsymptom development (pain) in the asymptomatic contralateral hip of patientswith DDH undergoing unilateral joint-preserving surgery? (2) Is the center gapmeasurement associated with OA progression or symptom development in thesehips? (3) Is the center gap measurement correlated with previous radiographicparameters?
METHODS:
A total of 297 patients (319hips) underwent unilateral eccentric rotational acetabular osteotomy at ourinstitution between July 1989 and December 1999. We performed no otherjoint-preserving surgery to treat patients with DDH during this timeframe. Theinclusion criteria for the study were patients younger than 55 years of age,the contralateral hip classified as Tönnis Grade 0, no previous surgicalinterventions, and asymptomatic at the time of eccentric rotational acetabularosteotomy (155 patients, 155 hips). The exclusion criteria were a contralateralhip without dysplasia (four patients, four hips), loss to followup before 10years (42 patients, 42 hips [27%]), or missing medical records or radiographs(21 patients, 21 hips [14%]). The remaining 88 patients (88 hips; 11 males and77 females) with a mean age of 39 years (range, 17-53 years) and mean followupof 20 years (range, 10-27 years) were analyzed. From the institutionaldatabase, radiographic parameters including the center gap in the AP view wereassessed using radiographs at the time of eccentric rotational acetabularosteotomy, and the Tönnis grade was recorded 1 year postoperatively andannually thereafter retrospectively. We defined migration of the rotationalcenter of the femoral head based on the rotational center of the acetabulum inthe horizontal plane as center gap X (mm) and in the vertical plane as centergap Y (mm) and defined the absolute value between the centers as center gapdistance (mm). Using κ statistics, intra- and interobserverreliabilities were determined to be 0.896 and 0.857 for center gap X, 0.912 and0.874 for center gap Y, and 0.912 and 0.901 for the center gap distance, respectively.When patients reported any contralateral ipsilateral hip pain during clinicvisits, the hip was considered symptomatic. Kaplan-Meier survivorship analyseswere performed with OA progression or symptom development in the nonoperativehip as the endpoint. Multivariate analyses were performed to assess riskfactors for each outcome using the Cox proportional hazards model. Correlationanalyses between the center gap and other parameters including lateralcenter-edge angle, femoral head extrusion index, acetabular depth-to-widthindex, femoral head lateralization, minimum width of the joint space, headsphericity, and joint congruency were performed using Pearson's correlationcoefficient.
RESULTS:
At 20 years postoperatively,the probability of OA progression in the nonoperative hip was 13% (95%confidence interval [CI], 7.1-22.1) and the probability of symptom developmentwas 34% (95% CI, 24.7-46.1). The center gap X measurements in the groups withOA progression (lateral 2.0 ± 2.1 [SD] mm) or symptom development(lateral 0.9 ± 2.4 mm) took a more lateral directionthan those in the group without OA progression (medial 0.4 ± 2.1 mm) or symptom development (medial 0.5 ± 2.0 mm) (OA progression, p < 0.001; symptom development, p =0.005). The center gap Y measurements in the groups with OA progression (distal2.7 ± 7.1 mm) or symptom development (distal 2.1 ± 6.0 mm) took a more distal direction than those in the groupwithout OA progression (proximal 1.6 ± 6.2 mm) orsymptom development (proximal 2.5 ± 6.1 mm) (OAprogression, p = 0.027; symptom development, p = 0.001). Independent riskfactors for OA progression were the femoral head extrusion index (hazard ratio[HR], 1.11; 95% CI, 1.01-1.22; p = 0.028) and the center gap X (HR, 1.52; 95%CI, 1.07-2.16; p = 0.019), whereas no independent risk factors for symptomdevelopment were found. The center gap in the horizontal plane had nocorrelations with any other radiographic parameter studied.
CONCLUSIONS:
The center gap in thehorizontal plane had a modest association with OA progression in this group ofpatients with DDH. Future studies are needed to determine the normal value of the center gap for patients without DDH and to assess the center gap in lateralradiographic views.
文献出处:Morita D, Hasegawa Y, Seki T,Amano T, Takegami Y, Kasai T, Higuchi Y, Ishiguro N. A Possible NewRadiographic Predictor of Progression of Osteoarthritis inDevelopmentalDysplasia of the Hip: The Center Gap. Clin Orthop Relat Res. 2018Nov;476(11):2157-2166. doi: 10.1097/CORR.0000000000000458.



 京公网安备11010502051256号
京公网安备11010502051256号