髋膝文献精译荟萃(第3期)
2018-05-26 文章来源:304关节学术 点击量:1963 我要说
第一部分:关节置换相关文献
文献1
全膝关节置换术后的髌骨低位是真正的髌骨低位吗?
译者:张轶超
将假体植入膝关节后,髌骨和胫骨垫片之间的距离变小有两种可能,即髌骨下移和关节线抬高。前者被称为髌骨低位。而后者的髌骨相对于股骨的位置是正常的,所以被称为假性髌骨低位。由于髌骨低位是因髌腱短缩造成的,而假性髌骨低位是由于关节线的抬高所导致,所以对于这两种情况的治疗方法是不同的。相比假性髌骨低位,在真性低位的翻修术中,外翻髌骨及伸膝装置比较困难。重要的是不要想只通过计算关节的Blackburne-Peel 或 the Caton-Deschamps比率来确定是否存在髌骨低位,由于受到关节线位置变化的影响这些数据经常会误导我们。
Patella Baja After Total Knee Arthroplasty: Is It Really Patella Baja?
In the prosthetic knee, narrowing of the space between the patella and the tibial polyethylene can be due to distal positioning of the patella or to a proximal transfer of the joint line. In the former case, one is dealing with patella baja. In the latter case, the patella is in its normal position relative to the femur, a situation we call pseudo–patella baja. The therapeutic options for patella baja and pseudo–patella baja are different because the former is due to a short patellar tendon, and the latter is due to a raised joint line. Eversion of the extensor mechanism during revision surgery may be more challenging with true patella baja compared with pseudopatella baja. It is important not to attempt to detect true patella baja with either the Blackburne-Peel or the Caton-Deschamps ratio in the setting of a prosthetic knee because these ratios are affected adversely by the position of the joint line.
文献出处:Grelsamer RP.Patella baja after total knee arthroplasty: is itreally patella baja?J Arthroplasty. 2002 Jan;17(1):66-9.
文献2
全髋关节置换术后站立位片上测量的髋臼和股骨假体前倾角在传统定义的假体安全区范围外
译者:马云青
背景:多数髋关节置换术后脱位发生在站立位或坐位时,但对于假体角度安全区的定义是在仰卧位。我们的目标是定位患者术前和术后骨盆和髋关节的方向,明确在仰卧位定义的假体安全区角度是否可用于评估术后站位X线片。
方法:对66例全髋关节置换术患者的术前、术后3D-EOS图像进行评估。所有患者在随访期内无假体脱位(随访时间12-36个月)。测量髋臼假体前倾角(含前骨盆平面[APP]和患者功能平面)和股骨假体倾角。同时测量骶骨斜度、骨盆前倾角、骨盆倾斜角及骨盆投射角。
结果:术后在APP和患者功能平面,髋臼前倾角均增加(P<.001)。股骨颈前倾角在术后减少(P=.0942)。术前骶骨斜度为42.4°(-25.9°至 24°),术后为40.3°(-4.1°至 64.2°) (P=.013)。骨盆前倾角从术前15.2°(10.4°至 43.8°)变为术后17.2°(-6°至 46.7°) (P=0.008)。骨盆倾斜度从术前的1.12°(-25.9°至 24°)变为术后的-1.2°(-40.7°至 23.4°)(P=,005)。
结论:站立位时多数患者的髋臼和股骨假体角度在安全范围以外。 在大多数患者中,由于骨盆前后倾斜导致前骨盆平面(APP)在站立位不是垂直的。对于站立位骨盆严重前倾或后倾的患者,应用以仰卧位定义的假体安全角度范围是不适当的。
Acetabular andFemoral Anteversions in Standing Position are Outside the Proposed Safe ZoneAfter Total Hip Arthroplasty
Background: Although most hip dislocations occur in either standing or sitting position, the safe zone for implant position is defined for the supine position. Our goal was to determine preoperative and postoperative pelvis and hip orientations and whether the safe zone defined in supine position can be used to assess standing radiographs.
Methods: Preoperative and postoperative three-dimensional EOS images were assessed in 66 total hip arthroplasty patients. None of the patients had dislocation within the follow-up period (12-36 months). The acetabular anteversion (both anterior pelvic plane [APP] and patient functional plane) and the femoral anteversion were measured. The sacral slope, pelvic version, pelvic inclination, and pelvic incidence were also measured.
Results: Acetabular anteversion increased postoperatively in both APP and patient functional plane (P <.001). Femoral neck anteversion decreased postoperatively (P=.0942). Sacral slope was 42.4° (-25.9° to 24°)preoperatively compared with 40.3° (-4.1° to 64.2°) postoperatively (P=.013). Pelvic version changed from 15.2° (-10.4° to 43.8°) to 17.2° (-6° to 46.7°;P=0.008). Pelvic inclination was 1.12° (-25.9° to 24°) before total hip atptnroplasty and -1.2° (-40.7° to 23.4°) postoperatively (P=.005).
Conclusion: The acetabular and femoral implant orientations in standing position reside out of the safe zone in most patients. The APP is not vertical in standing position in most patients due to anterior or posterior pelvic tilt. The proposed safe zone in supine position may not be a useful measure in the assessment of standing radiographs of patients with significant anterior or posterior pelvic tilt.
文献出处:Lazennec JY, Thauront F, Robbins CB, Pour AE. Acetabular and Femoral Anteversionsin Standing Position are Outside the Proposed Safe Zone After Total Hip Arthroplasty. J Arthroplasty. 2017 Nov;32(11):3550-3556.
文献3
截骨缩平台技术与拉花松解技术在内翻膝全膝置换术中的效果对比:前瞻性随机对照试验
译者:张蔷
背景:比较内翻膝全膝置换术中应用截骨缩平台技术与拉花松解技术对间隙的改变,分别比较屈曲间隙和伸直间隙的改变以及总体成功率。
方法:本研究共纳入106例内翻膝,要求术中简单松解后内外侧间隙差距≥3mm。将患者随机分配至截骨缩平台组和拉花松解组,各53例。接下来进行截骨缩平台松解和拉花松解。分别记录屈曲和伸直间隙变化,以及两种方法的松解成功率。
结果:伸直间隙变化分别为:截骨缩平台技术3.5 ± 0.5 mm V.S. 拉花松解技术 2.3 ± 0.8 mm。屈曲间隙变化分别为:截骨缩平台技术1.1 ± 0.5 mm V.S. 拉花松解技术 2.3 ± 1.2 mm。总体成功率:截骨缩平台技术90.6% V.S. 拉花松解技术67.9%。
结论:作为内翻膝的松解方法,截骨缩平台技术在松解伸直间隙不平衡方面更有效,而拉花松解技术在松解屈曲间隙不平衡方面更有效。总体成功率截骨缩平台技术高于拉花松解技术。
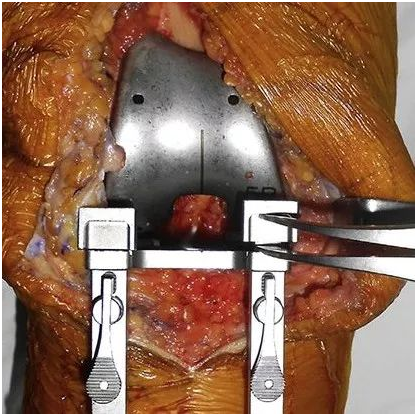
用间隙测量器测试内外侧间隙差距
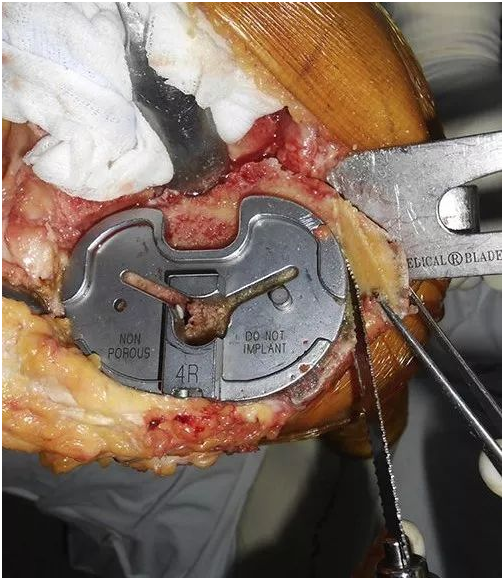
截骨缩平台(每2mm一次,截骨后再次测试间隙差距直至小于3mm,不够则继续截骨;若已至缩平台极限仍未达标则标记为失败,继续使用拉花进行剩余松解)
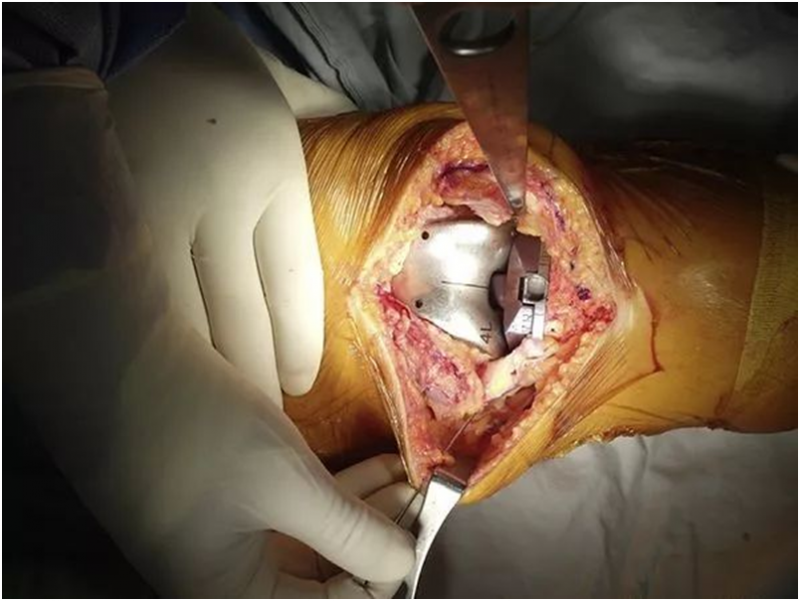
拉花松解(使用19号针头在伸直位施以外翻应力下穿刺MCL,每穿10次为一组,每组后再次测试间隙差距,若小于3mm则为成功,若10组后仍未小于3mm则标记为失败,继续使用截骨缩平台进行余下的松解)
Reduction Osteotomy VS Pie-Crust Technique as Possible Alternatives for Medial Release in Total Knee Arthroplasty and Compared in a Prospective Randomized Controlled Trial
Background: To compare the gap change between the pie-crust technique and reduction osteotomy to determine their effects on flexion and extension gaps and their success rates in achieving ligament balancing during total knee arthroplasty.
Methods: In a prospective randomized controlled trial, 106 total knee arthroplasties were allocated to each group with 53 cases. If there was a narrow medial gap with an imbalance of ≥3 mm after the initial limited medial release, either reduction osteotomy or pie-crust technique was performed. The changes of extension and flexion medial gaps along with the success rate of mediolateral balancing were compared.
Results: There was a significant difference in the change of medial gap in knee extension with mean changes of 3.5 ± 0.5 mm and 2.3 ± 0.8 mm in the reduction osteotomy and pie-crust groups, respectively (P < .001). For flexion gap, greater change was found in the pie-crust group compared with the reduction osteotomy group; the mean medial gap changes in knee flexion were 1.1 ± 0.5 mm and 2.3 ± 1.2 mm in the reduction osteotomy and pie-crust groups, respectively. The success rates were 90.6% and 67.9% in reduction osteotomy and pie-crust groups, respectively (P=.007).
Conclusion: As an alternative medial release method, reduction osteotomy was more effective in extension gap balancing, and pie-crust technique was more effective in flexion gap balancing. The overall success rate of mediolateral ligament balancing was higher in the reduction osteotomy group than in the pie-crust group.
文献出处:Ahn JH, Yang TY, Lee JY. Reduction Osteotomy vs Pie-Crust Technique as Possible Alternatives for Medial Release in Total Knee Arthroplasty and Compared in a Prospective Randomized Controlled Trial. J Arthroplasty. 2016Jul;31(7):1470-5.
第二部分:保髋换相关文献
文献1
什么是Ratliff分型?
译者:罗殿中
概要:本研究根据71例儿童股骨颈骨折患者的临床特点,分别就其发生率、骨折分类、损伤机制、并发症发生情况及治疗等方面逐一总结与阐述。
发生率:成人股骨颈骨折发生率为儿童的130倍。儿童股骨颈骨折可以发生于3-17岁。
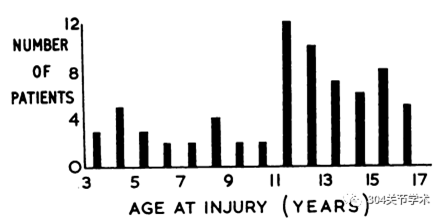
损伤年龄分布
分类:儿童股骨颈骨折可分为4类:经骺骨折、经颈骨折、股骨颈基底部骨折以及转子处骨折。
损伤机制:损伤原因多为严重暴力,本研究54例因严重暴力所致,包括高处坠落伤24例、车撞伤16例以及跌落伤14例。
诊断:未移位骨折或可漏诊,本研究21例未移位骨折中有2例在入院时漏诊。
并发症发生情况:儿童股骨颈骨折并发症发生率高(股骨头坏死发生率约42%)。
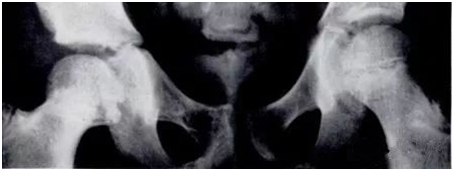
股骨头骨骺坏死:依据影像学密度改变可分为以下III型(见下图)。I型:高密度改变弥漫伴股骨头骨骺完全塌陷;II型:高密度改变局部伴股骨头骨骺轻微塌陷;III型:高密度改变局限于股骨颈处,未累及骨骺。本研究I型15例,II型、III型各7例。
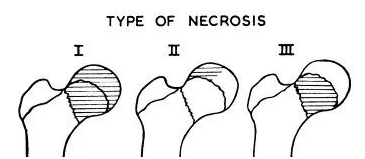
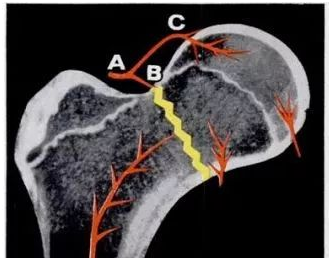
作者认为,儿童股骨头骨骺与股骨干骺端血运没有交通支。股骨头上支持带动脉为股骨头外上部骨骺的主要供支,圆韧带动脉为次要供支,仅供应骨骺内下部分。如果上支持带血运自起始部损伤(A处,见下图),将导致全骺端坏死(I型)。如果干骺端动脉分支损伤(B处)将导致干骺端坏死(III型)。如果上支持带血运自头颈交界处损伤(C处),将导致外上大部股骨头骨骺坏死(II型)。
本研究共30例(42%)发生股骨头骨骺坏死,包括26例移位骨折及4例未移位骨折。23例为经颈骨折,6例为股骨颈基底部骨折,另外1例骨折部位不明。需注意的是,成人股骨颈基底部骨折一般不会导致股骨头坏死,而本研究显示,儿童股骨颈基底部骨折可发生股骨头骨骺坏死。
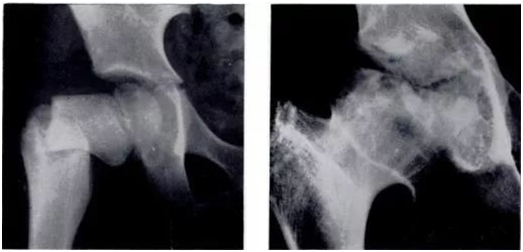
9岁儿童,车撞伤致右股骨颈基底部骨折,5年后发生股骨头坏死
延迟愈合或不愈合:本研究中17例患者出现延迟愈合,其中7例发展为骨折不愈合。
骨骺过早闭合:11例患者出现骨骺早闭。其中6例为股骨颈坏死后骨骺闭合。
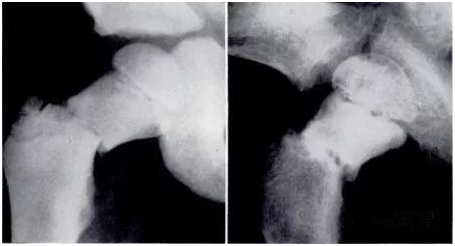
11岁儿童股骨颈骨折,3月后出现III型坏死,坏死位于股骨颈处,未累及股骨头骨骺
2年后,其右侧股骨头骨骺闭合
治疗:
非移位骨折:15例石膏固定、2例夹板固定、1例卧床休息无石膏或夹板固定、2例框架外固定以及1例切开内固定。
移位骨折:该类患者治疗效果不满意,仅不到三分之一的患者获得好的效果。具体治疗方法包括:闭合复位后石膏固定19例、闭合复位后内固定19例,复位后夹板固定3例、骨牵引下逐步复位1例、切开复位内固定1例、一期转子下截骨4例以及未治疗2例。其中近50%的闭合复位内固定患者可获好的效果。不推荐闭合复位石膏固定治疗移位骨折。
结论:
1、儿童股骨颈骨折少见,但可发生于3-16岁各个年龄段;
2、多由严重暴力因素所致,尤其多见于高处坠落伤或车撞伤;
3、股骨颈骨折后并发症多见,如无菌性坏死、延迟愈合、不愈合以及骨骺早闭所致的生长发育停止;
4、30例患者发生无菌性坏死(42%),包括3种分型(Ratliff分型);
5、移位型骨折预后差,49例患者中仅15例效果好。
原文无摘要,上文为对原文的概括总结,文献出处:A. H. C. RATLIFF. FRACTURES OF THE NECK OF THE FEMUR IN CHILDREN. THE JOURNAL OF BONE AND JOINT SURGERY. 1962;44B(3):528-542.
文献2
外翻型股骨头骺滑脱:关节运动的病理生理学变化和关节囊内复位手术的疗效
译者:程徽
实验目的:本研究的目的是:1. 报告一种由外翻型股骨头骺滑脱造成的特殊的髋关节撞击;2. 报告关节囊内复位手术治疗该疾病的疗效。
实验设计:病例系列研究。
实验设置:多中心。
纳入患者:选自6例外翻型股骨头骺滑脱患者纳入研究,共8髋。
手术干预:均进行关节囊内复位截骨术。其中,髋臼侧需要治疗的患髋同时进行了髋臼周围截骨术。
主要观察指标:临床转归和影像学转归,以及髋关节运动病理生理学变化。
结果:6例患者的8侧患髋中,5髋进行股骨头下截骨复位,3髋进行股骨颈截骨复位。内侧突出的干骺端造成了髋臼前壁包容性撞击,高位的外翻造成了头颈交界处后方的冲击性撞击。术前平均骺干角是110.5度(90-125度),术后改善为62度(55-70度)。在最后一次随访中,7髋无痛无撞击,关节活动范围正常。1髋在多次尝试复位失败后进行髋关节置换术。使用Merle d'Aubigne评分系统评价,5髋功能优(18-16分),2髋良(16-15分),1髋差(6分)。
结论:外展型股骨头骺滑脱畸形造成的撞击典型而复杂。解剖复位可以重建正常的关节形态,改善髋关节活动范围,得到满意的疗效。
Valgus Slipped Capital Femoral Epiphysis: Pathophysiology of Motion and Results of Intracapsular Realignment
OBJECTIVES: The purpose of this study was to report (1) a different but specific pattern of impingement in hips involved with valgus slipped capital femoral epiphysis (valgus SCFE) and (2) the results of surgical treatment using intracapsular realignment techniques.
DESIGN: Case series.
SETTING: Multiple academic centers.
PATIENTS: Six patients with 8 involved hips referred for valgus alignment of proximal femoral epiphysis (valgus SCFE).
INTERVENTION: Intracapsular realignment osteotomy combined with periacetabular osteotomy if needed.
MAIN OUTCOMEMEASUREMENT: The clinical and radiographical results and pathophysiology of motion.
RESULTS: Eight hips in 6 patients were treated with subcapital (5 hips) or femoral neck (3 hips) osteotomy for realignment. The medially prominent metaphysis created an inclusive impingement at the anterior acetabular wall, whereas the high coxa valga favored impacting impingement at the posterior head-neck junction. The mean preoperative epiphyseal-shaft angle of 110.5 (range 90-125 degrees) was reduced to 62 degrees (range 55-70 degrees) postoperatively. At the last follow-up, all but 1 hip were pain-free and impingement-free, with normal range of motion. One hip was replaced after repeated attempts of correction. The overall hip functional result using modified Merle d'Aubigne scoring system was excellent in 5 hips (18-16 points), good in 2 hips (16-15 points), and poor in 1 hip (6 points).
CONCLUSIONS: Impingement in valgus SCFE deformity is specific and complex. Anatomical realignment can lead to favorable results by the restoration of normal morphology and impingement-free range of motion.
文献出处:Kalhor M,Gharanizadeh K, Rego P, Leunig M, Ganz R. Valgus Slipped Capital Femoral Epiphysis: Pathophysiology of Motion and Results of Intracapsular Realignment. J Orthop Trauma. 2018 Feb;32 Suppl 1:S5-S11.
文献3
髋臼外侧覆盖对髋臼盂唇尺寸的预测
译者:肖凯
背景:髋关节骨性结构的异常通常与软组织结构异常伴随存在。如果能充分理解及定义这种伴随的改变,将会更好地指导临床。
目的:研究临床中接受保髋治疗患者的髋臼盂唇尺寸与髋臼外侧覆盖之间的关系。
方法:本试验为回顾性研究,我们选取了2013年6月至2015年6月间接受保髋治疗的236例患者做研究对象。按中心边缘角(LCEA)大小将患者分为4组,分别是正常覆盖组(25°-39.9°)、过度覆盖组(≥40°)、交界性发育不良组(20°-24.9°)及发育不良组(<20°)。术前进行髋关节核磁共振检查,对髋臼外侧、前方及前下方盂唇宽度进行测量。
结果:髋关节发育不良组及交界性发育不良组3个层面的盂唇宽度均明显大于正常覆盖组(P < .001)及过度覆盖组(P < .001)。有趣的是,髋关节发育不良组及交界性发育不良组的盂唇宽度却比较接近。在髋关节发育不良组、交界性发育不良组及正常覆盖组,髋臼外侧的盂唇最宽,前下方的盂唇最窄(P < .001)。在过度覆盖组,3个部位的盂唇宽度无明显差异。多变量分析显示,无论测量位置在哪,LCEA都是预测盂唇宽度最有效的指标。
结论:髋关节发育不良组及交界性发育不良组负重区的盂唇宽度增加,这可能是对于骨性结构缺失的代偿。盂唇的宽度可能反应关节的稳定情况,并对交界性髋关节发育不良的临床治疗方案提供数据支持。
Lateral Acetabular Coverage Predicts the Size of the Hip Labrum
BACKGROUND: Bony morphological abnormalities of the hip joint are often accompanied by adaptive soft tissue changes. These adaptive changes, if better understood and characterized, may serve to inform clinical decision making.
PURPOSE: To investigate the correlation between the size of the hip labrum and lateral acetabular coverage in patientsat our hip preservation clinic.
METHODS: A cohort of 236 patients seen at a dedicated hip preservation service between June 2013 and June 2015 were retrospectively analyzed. Patients were grouped according to the degree of acetabular coverage, as measured by the lateral center-edge angle (LCEA): normal acetabular coverage (25°-39.9°), acetabular overcoverage (≥40°), borderline dysplasia (20°-24.9°), and frank dysplasia (<20°). Preoperative magnetic resonance imaging was utilized to measure the length ofthe labrum at 3 locations: laterally, anteriorly, and anteroinferiorly.
RESULTS: Frankly dysplastic and borderline dysplastic hips exhibited larger values of labral length at all locations when compared with hips with normal acetabular coverage (P < .001) or acetabular overcoverage (P < .001). Interestingly, mean labral length values in frank dysplasia were statistically similar to corresponding measurements in borderline dysplasia. In hips with frank dysplasia, borderline dysplasia, or normal acetabular coverage, labral length was consistently greatest at the lateral labrum and correspondingly lowest at the anteroinferior labrum (P < .001). In hips with acetabular overcoverage, labral length did not vary significantly between the lateral, anterior, and anteroinferior locations. Multivariate analyses confirmed LCEA to be the strongest predictor of labral length, irrespective of measurement location.
CONCLUSION: Patients with borderline dysplasia and frank dysplasia exhibited increased values of labral length in the weight bearing zone, potentially indicating a compensatory reaction to the lack of bony coverage. Labral length may serve as an instability marker and inform clinical decision making for patients with borderline dysplasia.
文献出处:Garabekyan T, Ashwell Z, Chadayammuri V, Jesse MK, Pascual-Garrido C, Petersen B, Mei-Dan O. Lateral Acetabular Coverage Predicts the Size of the Hip Labrum. Am J Sports Med. 2016 Jun;44(6):1582-9.
文献4
青少年髋关节发育不良患者髋臼周围截骨术后耻骨坐骨连接处骨折情况分析
译者:张振东
背景:髋臼周围截骨术(periacetabular osteotom,PAO)可治疗成人髋关节发育不良,其手术疗效已被广泛认可。对于有症状的骨骼发育成熟的青少年患者,亦可行PAO治疗。术后髋关节局部应力的重新分布或可导致耻骨坐骨连接处骨折(ischio-pubic junction,IPJ)。
方法:本研究回顾性分析本中心1999年至2012年所有接受PAO治疗的青少年髋关节发育不良患者。术前、术后6周、术后1年均拍摄髋关节站立正位片,并分别测量外侧CE角、Sharp角、臼顶倾斜角等影像学指标,同时记录患者术后改良髋关节Harris评分。本研究排除手术时年龄大于21岁或随访小于2年的患者。
结果:166例患者(187髋)纳入该研究,患者年龄为15.6±2.5岁。共有12例患者(12髋)发生IPJ,占6.4%。其中7髋于术后即刻摄片时发现,其余5髋于术后6周随访时发现。7例(58.3%)骨折发生与坐骨截骨处不愈合有关。所有骨折患者中,6例(50%)在2年复查时愈合,另外6例仍未愈合。未发生IPJ患者与发生IPJ患者在术前、术后6周及末次随访时,外侧CE角(P=0.94, 0.29, 0.27)、Sharp角(P=0.95, 0.38, 0.16)、臼顶倾斜角(P=0.37, 0.21, 0.54)均无显著性差异。术后改良髋关节Harris评分两组间亦无差异。经分析骨折发生因素,Charcot-Marie-Tooth (CMT)病更易发生IPJ (P=0.001)。发生IPJ患者年龄更大(17.1 vs. 15.5, P=0.05)。两组患者性别分布无差异(P=0.22)。
结论:青少年髋关节发育不良患者PAO术后IPJ发生率为6.4%,部分患者可发生在术中。骨折发生与Charcot-Marie-Tooth (CMT)病及坐骨截骨处不愈合有关。IPJ并不影响PAO手术疗效且发生后并不需要手术治疗。
Fracture at theIschio-Pubic Junction After Periacetabular Osteotomy in the AdolescentPopulation
INTRODUCTION: The Ganz periacetabular osteotomy (PAO) is a well-accepted surgical intervention for hip dysplasia. In the adolescent population it is performed in patients who are skeletally mature with symptoms related to acetabular dysplasia. Redistribution of stresses through the hemipelvis after PAO can lead to a fracture at the ischio-pubic junction (IPJ).
METHODS: This is an IRB-approved, retrospective analysis of adolescent patients treated with a PAO for acetabular dysplasia from 1999 to 2012 at a single institution. Radiographic measurements were performed to include the lateral center-edge angle, Sharp acetabular index, and acetabular index of the weight-bearing zone. These were measured preoperatively and at 6-weeks and 1 year postoperatively from a standing anterior posterior pelvis radiograph. Postoperative modified Harris hip scores (mHHS) were also analyzed. Patients over the age of 21 at time of surgery and those with <2 years of follow-up were excluded.
RESULTS: One hundred sixty-six patients (187 operated hips) at an average age of 15.6±2.5 were included. Twelve (6.4%) fractures at the IPJ were identified in 12 patients. Seven were identified on the initial postoperative films, whereas 5 were identified after the 6-week visit. Seven (58.3%) fractures had an associated superior posterior ramus nonunion. Six (50%) healed by 2 years after surgery; the remaining 6 (50%) went on to nonunion. Compared with those without a fracture, there was no significant difference in preoperative, 6 weeks postoperative, and final center-edge angle (P=0.94, 0.29, 0.27), Sharp acetabular index (P=0.95, 0.38, 0.16), or AIBWZ (P=0.37, 0.21, 0.54). There was no difference in postoperative mean modified Harris hip scores (P=0.63). Analysis of predisposing factors demonstrated that patients with Charcot-Marie-Tooth (CMT) disease were more likely to develop an IPJ fracture (P=0.001). Patients with an IPJ fracture were older (17.1 vs. 15.5, P=0.05). There was no difference based on patient sex (P=0.22).
DISCUSSION AND CONCLUSIONS: The incidence of fracture at the IPJ after PAO in the adolescent population is 6.4% with some occurring at the time of surgery. These fractures are also associated with a nonunion at the superior posterior ramus cut and an underlying diagnosis of Charcot-Marie-Tooth. These fractures are not clinically significant and in this series did not merit further intervention when identified.
文献出处:Swann M, Sucato DJ, Romero J, Podeszwa DA.Fracture at the Ischio-Pubic Junction After Periacetabular Osteotomy in the Adolescent Population. J Pediatr Orthop. 2017Mar;37(2):127-132.
文献5
发育性髋关节发育不良筛查
译者:杨金鑫
髋关节发育不良的筛查一直是个有争议的话题。筛查的方法可以是物理检查(Ortolani法或Barlow法),外加髋部超声影像检查(选择性检查存在高危因素的患儿还是检查所有新生儿)。在英国,NIPE指南推荐对所有新生儿行髋部物理检查,全科医生对6-8周龄的新生儿行髋部体检,对4-6周龄存在易患因素的新生儿行髋部超声检查,用以确定DDH。强调了英国现行筛查政策(物理检查和超声检查)的有效性和困难性。本研究的目的是根据10年或以上的纵向队列研究,对DDH的易患因素和诊断方法的有效性进行评估。
结论:DDH筛查不符合世界卫生组织大多数有效筛查的标准,并且由于其灵敏度和阳性预测值(PPV)低,仅被认为有监测作用。DDH筛查存在过度诊断和过度治疗的重大风险。国际上对DDH筛查仍存在分歧。DDH患者主要为女性,故女性被认为是易患因素。全科医生的筛查中极少有男性DDH患者。全科医生对6-8周龄新生儿行髋关节体检阳性检出率非常低,并且此种方法的筛查诊断存在不确定性。单侧髋关节外展受限与新生儿生长发育的时间存在相关性,它在DDH的诊断中是一种有用的临床体征。大多数以前被认为是“易患因素”的因素并不是真正的易患因素,这些因素与DDH几乎没有联系。
Screening inDevelopmental Dysplasia of the Hip
Screening for Developmental Dysplasia of the Hip (DDH) is a controversial subject. Screening may be by universal neonatal clinical examination (Ortolani or Barlow manoeuvres) with the addition of sonographic imaging of the hip (selective 'at risk' hips or universal screening in the neonate). In the UK, the NIPE guidelines recommend universal neonatal clinical assessment of the hip joints, a General Practitioner 6-8 week clinical 'hip check' and assessment clinically with sonographic imaging at 4-6 weeks for certain 'at risk' hips for pathological DDH. The effectiveness and difficulties arising from the UK current screening policy (clinical and sonographic) are highlighted. The purpose of the review was to assess the risk factors and efficacy of diagnostic methods in DDH, based on longitudinal cohort studies of 10 years or more.
CONCLUSION: Hip screening in DDH does not meet most of the World Health Organisation's criteria for an effective screening programme and should only be considered as surveillance due to its low sensitivity and positive predictive value (PPV). There is a significant risk of over diagnosis and over treatment. There is no International consensus on screening in DDH. Pathological DDH is mainly a female condition and 'at risk'/General Practitioner screening identifies few pathological cases in male subjects. The General Practitioner 6-8 week 'hip check' has a very low PPV for pathological DDH and is of doubtful value in screening and diagnosis. Unilateral limitation of hip abduction is a time dependent and useful clinical sign in the diagnosis of pathological DDH. The majority of the previously considered 'at risk' factors are not true risk factors with little or no association with pathological DDH.
文献出处:PatonRW. Screening in Developmental Dysplasia of the Hip (DDH). Surgeon. 2017.15(5): 290-296.



 京公网安备11010502051256号
京公网安备11010502051256号