第六届中国国际腰椎外科学术会议第三轮通知
2014-01-29 文章来源:骨科在线 我要说
骨科在线版权所有,如需转载请注明来自本网站.
尊敬的各位同仁:
中国康复医学会脊柱脊髓专业委员会腰椎研究学组
第六届中国国际腰椎外科学术会议组委会


附:第六届中国国际腰椎外科学术会议九大议题
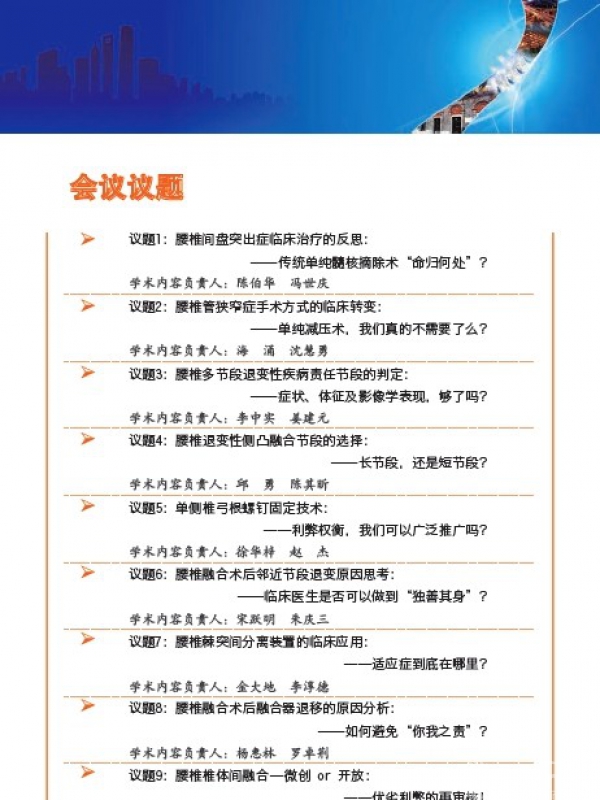
议题1:腰椎间盘突出症临床治疗的反思:
----传统单纯髓核摘除术“命归何处”?
本章节内容负责人:陈伯华教授 冯世庆教授
自1934年Mixter和Barr明确坐骨神经痛与腰椎间盘突出之间的密切关系【1】,单纯髓核摘除术治疗腰椎间盘突出症已有近80年历史,至今仍是治疗腰突症最常用的经典术式【2】。美国每年大约有30万腰突症患者接受单纯髓核摘除治疗【3】,大量的文献资料表明其长期随访的优良率高达87-98%【4-6】。尽管相关研究认为只有极少数的单纯髓核摘除术需要辅以内植物【6-8】,且有研究提示其并不能明显提高临床疗效【9】。但近几年来,随着各种脊柱内植物系统的不断研发,采用减压附加内植物技术治疗腰椎间盘突出症越来越普遍。对于这一现象我们是不是需要进行一定的反思呢?
1. Mixter, WJ, and Barr, JS: Rupture of the Intervertebral Disc with Involvement of Spinal Canal. New England Jour. Med., I934, 211: 2I-215.
2. Henriksen L, Schmidt K, Eskesen V, Jantzen E: A controlled study of microsurgical versus standard lumbar discectomy. Br J Neurosurg., 1996,10:289-293,.
3. Bruske-Hohlfeld I, Merritt JL, Onofrio BM, Stonnington HH, Offord KP,Bergstralh EJ, Beard CM, Melton LJ 3rd, Kurland LT: Incidence of lumbar disc surgery. A population-based study in Olmsted County, Minnesota, 1950–1979.Spine, 1990,15:31–35,.
4. Yorimitsu E, Chiba K, Toyama Y, et al. Long-term outcomes of standard discectomy for lumbar disc herniation: a follow-up study of more than 10 years. Spine, 2001,26(6):652-657.
5. Buttermann GR. Treatment of lumbar disc herniation: Epidural steroid injection compared with discectomy - A prospective, randomized study. J Bone Joint Surg Am. Apr 2004;86A(4):670-679.
6. Clinical Guidelines for Multidisciplinary Spine Care Diagnosis and Treatment of Lumbar Disc Herniation with Radiculopathy. Copyright © 2012 North American Spine Society ISBN 1-929988-32-X. http://www.spine.org/Documents/LumbarDiscHerniation.pdf
7. Bambakidis NC, et al. Indications for surgical fusion of the cervical and lumbar motion segment. Spine.2005;30:S2-S6
8. Lalane LB, Marcuson KW. Adjacent segment disease of the lumbar spine: genetic versus biomechanical theories. COLUNA/COLUMNA, 2008, 7(3): 276-280.
9. Donceel P, Du Bois M. Fitness for work after surgery for lumbar disc herniation: a retrospective study. Eur Spine J.1998;7(1):29-35.
议题2:腰椎管狭窄症手术方式的临床转变:
----单纯减压术,我们真的不需要了么?
本章节内容负责人:海涌教授 沈慧勇教授
众所周知,彻底而有效的神经减压是腰椎管狭窄症患者手术治疗的第一要务;但同时需要兼顾脊柱的稳定性。生物力学研究显示减压范围的大小与术后节段稳定性存在明确的相关性。因此,在确保疗效的前提下,应尽量进行有限而精准的减压,维持手术节段的稳定性【1-4】。近年来,NASS(北美脊柱外科学会,North American Spine Society)、AAOS(美国骨科医师协会,American Academy of Orthopaedic Surgeons)等学术组织先后指出:对于下肢症状为主且不伴有节段失稳的腰椎管狭窄症患者手术治疗首选单纯减压术【4-7】;Weinstein等【8】进行的一项腰椎管狭窄症患者临床随机队列研究中88%的手术治疗患者采用单纯减压治疗,术后随访4年临床疗效良好。而国内关于腰椎管狭窄症临床诊疗指南进行的专家调查问卷最新结果显示:对于不伴有节段失稳的单纯中央管狭窄患者,72.1%的脊柱外科专家首选后路椎板切除减压融合内固定术。面对上述国内外腰椎管狭窄症临床手术治疗选择的巨大差异,您认为:单纯减压术,我们真的不需要了么?
1. 杨惠林, 马宏庆, 王根林, 等. 全国腰椎退行性疾患座谈会会议纪要. 中华骨科杂志; 2006,26(10): 711-716.
2. Thomé C, Zevgaridis D, Leheta O, et al. Outcome after less-invasive decompression of lumbar spinal stenosis: a randomized comparison of unilateral laminotomy, bilateral laminotomy, and laminectomy[J]. Journal of Neurosurgery: Spine, 2005, 3(2): 129-141.
3. Slätis P, Malmivaara A, Heliövaara M, et al. Long-term results of surgery for lumbar spinal stenosis: a randomised controlled trial. European spine journal, 2011, 20(7): 1174-1181.
4. Issack PS, Cunningham ME, Pumberger M, et al. Degenerative lumbar spinal stenosis: evaluation and management. J Am Acad Orthop Surg. 2012;20(8):527-35.
5. Watters WC 3rd, Baisden J, Gilbert TJ, etal; North American Spine Society. Degenerative lumbar spinal stenosis: an evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spinal stenosis. Spine J. 2008;8(2):305-10.
6. Clinical Guidelines for Multidisciplinary Spine Care Diagnosis and Treatment of Degenerative Lumbar Spinal Stenosis. Copyright © 2011 North American Spine Society. ISBN 1-929988-29-X. http://www.spine.org/Documents/LumbarStenosis11.pdf.
7. Kreiner DS, Shaffer WO, Baisden JL, et al. An evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spinal stenosis (update). Spine J. 2013 Jul;13(7):734-43.
8. Weinstein JN, et al. Surgical versus nonoperative treatment for lumbar spinal stenosis four-year results of the spine patient outcomes research trial. Spine, 2010, 35(14):1329-1338.
议题3:腰椎多节段退变性疾病责任节段的判定:
----症状、体征及影像学表现,够了吗?
本章节内容负责人:李中实教授 姜建元教授
腰椎多节段退变性疾病,临床表现多以间歇性跛行、腰背痛及下肢放射痛为主【1,2】。由于该疾病多见于老年患者,因此较高的围手术期并发症往往限制了大范围减压手术的实施【3】,也导致了腰椎多节段退变性疾病往往预后不佳的局面。为了解决这一问题,部分学者提出了选择性减压的概念【4,5】,但由于即使是目前NASS所推荐的MRI及CT等腰椎多节段退变性疾病首选的检查方法【6】,其诊断敏感性也仅为70-85%【7,8】,故对于部分患者仍然难以明确责任节段或部位,从而导致在多项前瞻性的随机对照研究中选择性减压技术并未能较广泛性减压获得更好的临床效果【9,10】。那么,您认为:目前应用于临床的神经电生理检查、选择性神经根阻滞及椎间盘造影,关节突关节封闭及特殊体检等方法在明确腰椎多节段退变性疾病的责任节段方面存在应用价值吗?
1. Park DK, An HS, Lurie JD, Zhao W, Tosteson A, Tosteson TD, Herkowitz H, Errico T, Weinstein JN.Does multilevel lumbar stenosis lead to poorer outcomes?: a sub-analysis of the Spine Patient Outcomes Research Trial (SPORT) lumbar stenosis study.Spine (Phila Pa 1976). 2010, 35(4):439-446.
2. Jensen MC, Brant-Zawadzki MN, Obuchowski N, et al. Magnetic resonanceimaging of the lumbar spine in people without back pain. N Engl J Med1994;331:69 –73.
3. Cassinelli EH, Eubanks J, Vogt M, Furey C, YooJ,Bohlman HH. Risk factors for the development of perioperative complications in elderly patients undergoing lumbardecompression and arthrodesis for spinal stenosis: ananalysis of 166 patients. Spine (Phila Pa 1976) 2007;32:230-5.
4. Matsui H, Tsuji H, Sekido H, Hirano N, Katoh Y, Makiyama N. Results of expansive laminoplasty for lumbar spinal stenosis in active manual workers. Spine (Phila Pa 1976)1992;17(3 Suppl):S37-40.
5. Postacchini F, Cinotti G, Perugia D, Gumina S. The surgical treatment of central lumbar stenosis: multiple laminotomy compared with total laminectomy. J Bone Joint Surg Br1993;75:386-92.
6. Watters WC 3rd, Baisden J, Gilbert TJ, Kreiner S, Resnick DK, Bono CM, Ghiselli G, Heggeness MH, Mazanec DJ, O'Neill C, Reitman CA, Shaffer WO, Summers JT, Toton JF; North American Spine Society.Degenerative lumbar spinal stenosis: an evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spinal stenosis.Spine J. 2008;8(2):305-310
7. Kent DL, Haynor DR, Larson EB, Deyo RA. Diagnosis of lumbar spinal stenosis in adults: a metaanalysis of the accuracy of CT, MR, and myelography. AJR Am J Roentgenol.1992;158(5):1135-44.
8. Bischoff RJ, Rodriguez RP, Gupta K, et al. A comparison of computed tomography-myelography, magnetic resonance imaging,and myelography in the diagnosis of herniated nucleus pulposus and spinal stenosis.J Spinal Disord. 1993;6(4):289-95.
9. Smorgick Y, Park DK, Baker KC, Lurie JD, Tosteson TD, Zhao W, Herkowitz HN, Fischgrund JS, Weinstein JN.Single- versus multilevel fusion for single-level degenerative spondylolisthesis and multilevel lumbar stenosis: four-year results of the spine patient outcomes research trial.Spine (Phila Pa 1976). 2013 May 1;38(10):797-805.
10. Seong YJ, Lee JS, Suh KT, Kim JI, Lim JM, Goh TS.Posterior decompression and fusion in patients with multilevel lumbar foraminal stenosis: a comparison of segmental decompression and wide decompression.Asian Spine J. 2011 Jun;5(2):100-6.
议题4:腰椎退变性侧凸融合节段的选择:
----长节段,还是短节段?
本章节内容负责人:邱勇教授 陈其昕教授
长期以来,融合节段的选择一直是腰椎退变性侧凸手术治疗中最富争议的问题之一【1-4】。多数学者认为矫正畸形并非该类患者手术治疗的主要目标,从而主张进行有限减压联合短节段融合【3-5】。但部分临床研究显示对于短节段融合术后存在畸形迅速进展、临床疗效不佳及短时间内二次手术等潜在问题【3-7】。由此部分学者尝试采用长节段融合以降低或避免上述问题的发生,但长节段融合存在创伤大、手术时间长、并发症多、费用昂贵等诸多不足,而且有研究显示长节段融合同样存在诸如邻近节段退变、矢状位整体失平衡、内固定失败等问题与不足【3, 8-10】。由此可知,对于腰椎退变性侧凸患者手术方案的选择绝不能一概而论,而应在明确不同方案应用指征的基础上综合考虑。那么,对于长节段与短节段融合的临床应用指征究竟如何把握呢?
1. Gupta MC. Degenerative scoliosis. Options for surgical management. Orthop Clin North Am. 2003;34(2):269-79.
2. Aebi M. The adult scoliosis. Eur Spine J. 2005 Dec;14(10):925-48.
3. Silva FE, Lenke LG. Adult degenerative scoliosis: evaluation and management. Neurosurg Focus. 2010;28(3):E1.
4. Cho KJ, Suk SI, Park SR, et al. Short fusion versus long fusion for degenerative lumbar scoliosis. Eur Spine J. 2008;17(5):650-6.
5. Schwarzenbach O. Short segment treatment of adult degenerative scoliosis with TLIF L3/L4. Eur Spine J. 2011;20(3):510-1.
6. Hwang DW, Jeon SH, Kim JW, et al. Radiographic progression of degenerative lumbar scoliosis after short segment decompression and fusion. Asian Spine J. 2009;3(2):58-65.
7. Kasliwal MK, Smith JS, Shaffrey CI, et al. Does prior short-segment surgery for adult scoliosis impact perioperative complication rates and clinical outcome among patients undergoing scoliosis correction? J Neurosurg Spine. 2012;17(2):128-33.
8. Cho KJ, Suk SI, Park SR, et al. Risk factors of sagittal decompensation after long posterior instrumentation and fusion for degenerative lumbar scoliosis. Spine (Phila Pa 1976). 2010;35(17):1595-601.
9. Ha KY, Son JM, Im JH, et al. Risk factors for adjacent segment degeneration after surgical correction of degenerative lumbar scoliosis.Indian J Orthop. 2013;47(4):346-51.
10. OʼShaughnessy BA, Bridwell KH, Lenke LG, et al. Does a long-fusion "T3-sacrum" portend a worse outcome than a short-fusion "T10-sacrum" in primary surgery for adult scoliosis? Spine (Phila Pa 1976). 2012;37(10):884-90.
议题5:单侧椎弓根螺钉固定技术:
----利弊权衡,我们可以广泛推广吗?
本章节内容负责人:徐华梓教授 赵杰教授
随着腰椎固定材料与固定技术的不断发展,上世纪90年代部分学者尝试采用单侧椎弓根螺钉固定以降低内固定应力、减少医源性损伤并降低医疗费用【1-2】。随后国内外多位学者对单边固定进行了临床研究,初步结论认为:单边固定的临床疗效、并发症发生率与传统双侧固定相当,同时具有创伤小、出血少、费用低等潜在优点【3-11】。然而,不少学者对单边固定能否提供手术节段融合所需的力学稳定性始终心存疑虑;部分临床研究显示单边固定远期存在一定不足【12-17】。而且单边固定技术的开展需要具备良好的椎体间融合操作技巧。基于以上利弊分析,结合您的临床实际经验,您认为:单边固定技术,我们可以广泛推广吗?(2min)
1. Hambly MF, Wiltse LL, Peek RD, et al. Unilateral lumbar fusion. Spine (Phila Pa 1976). 1991;16(6 Suppl):S295-7.
2. Suk KS, Lee HM, Kim NH, et al. Unilateral versus bilateral pedicle screw fixation in lumbar spinal fusion. Spine (Phila Pa 1976). 2000;25(14):1843-7.
3. Deutsch H, Musacchio MJ Jr. Minimally invasive transforaminal lumbar interbody fusion with unilateral pedicle screw fixation. Neurosurg Focus. 2006;20(3):E10.
4. Tuttle J, Shakir A, Choudhri HF. Paramedian approach for transforaminal lumbar interbody fusion with unilateral pedicle screw fixation. Technical note and preliminary report on 47 cases. Neurosurg Focus. 2006;20(3):E5.
5. Kim JG, Jin YJ, Chung SK,et al. Unilateral augmented pedicle screw fixation for foraminal stenosis. J Korean Neurosurg Soc. 2009;46(1):5-10.
6. Kasai Y, Inaba T, Kato T, et al.Biomechanical study of the lumbar spine using a unilateral pedicle screw fixation system. J Clin Neurosci. 2010;17(3):364-7.
7. Feng ZZ, Cao YW, Jiang C, et al. Short-term outcome of bilateral decompression via a unilateral paramedian approach for transforaminal lumbar interbody fusion with unilateral pedicle screw fixation. Orthopedics. 2011;34(5):364.
8. Xue H, Tu Y, Cai M. Comparison of unilateral versus bilateral instrumented transforaminal lumbar interbody fusion in degenerative lumbar diseases. Spine J. 2012;12(3):209-15.
9. Xie Y, Ma H, Li H, et al. Comparative study of unilateral and bilateral pedicle screw fixation in posterior lumbar interbody fusion. Orthopedics. 2012;35(10):e1517-23.
10. Mao L, Chen GD, Xu XM, et al. Comparison of lumbar interbody fusion performed with unilateral or bilateral pedicle screw. Orthopedics. 2013;36(4):e489-93.
11. Lin B, Xu Y, He Y, et al. Minimally invasive unilateral pedicle screw fixation and lumbar interbody fusion for the treatment of lumbar degenerative disease. Orthopedics. 2013;36(8):e1071-6.
12. Yücesoy K, Yüksel KZ, Baek S, et al. Biomechanics of unilateral compared with bilateral lumbar pedicle screw fixation for stabilization of unilateral vertebral disease. J Neurosurg Spine. 2008 Jan;8(1):44-51.
13. Aoki Y, Yamagata M, Nakajima F, et al. Posterior migration of fusion cages in degenerative lumbar disease treated with transforaminal lumbar interbody fusion: a report of three patients. Spine (Phila Pa 1976). 2009;34(1):E54-8.
14. Aoki Y, Yamagata M, Nakajima F, et al. Examining risk factors for posterior migration of fusion cages following transforaminal lumbar interbody fusion: a possible limitation of unilateral pedicle screw fixation. J Neurosurg Spine. 2010;13(3):381-7.
15. Rihn JA. Commentary: is bilateral pedicle screw fixation necessary when performing a transforaminal lumbar interbody fusion? An analysis of clinical outcomes, radiographic outcomes, and cost. Spine J. 2012;12(3):216-7.
16. Aoki Y, Yamagata M, Ikeda Y, et al. A prospective randomized controlled study comparing transforaminal lumbar interbody fusion techniques for degenerative spondylolisthesis: unilateral pedicle screw and 1 cage versus bilateral pedicle screws and 2 cages.J Neurosurg Spine. 2012;17(2):153-9.
17. Choi UY, Park JY, Kim KH, et al. Unilateral versus bilateral percutaneous pedicle screw fixation in minimally invasive transforaminal lumbar interbody fusion. Neurosurg Focus. 2013;35(2):E11.
议题6:腰椎融合术后邻近节段退变原因思考:
----临床医生是否可以做到“独善其身”?
本章节内容负责人:宋跃明教授 朱庆三教授
近年来,腰椎融合术后邻近节段退变问题越来越受到国内外广大脊柱外科医生的关注。关于腰椎融合术后邻近节段退变的确切原因,目前尚存在巨大争议[1]。诚然,腰椎融合改变了邻近节段的应力分布[2],但将邻近节段退变完全归咎于上述生物力学因素却有失偏颇;部分学者认为邻近节段退变与脊柱本身的自然退变密不可分[3-5];而现有的部分临床研究显示腰椎融合术中一些操作性因素对邻近节段退变的发生具有不容忽视的影响[6-12]。那么,腰椎融合术后邻近节段退变的发生:究竟是病程之责(退变的自然进程),还是融合之过(邻近节段应力改变)?除此之外,我们临床医生的一些操作性因素是否也起到了“推波助澜”的作用?你我是否能够完全做到“独善其身”呢?
1. Lalane LB, Marcuson KW. Adjacent segment disease of the lumbar spine: genetic versus biomechanical theories. COLUNA/COLUMNA, 2008, 7(3): 276-280.
2. Rao RD, David KS, Wang M. Biomechanical changes at adjacent segments following anterior lumbar interbody fusion using tapered cages. Spine, 2005, 30(24): 2772-6.
3. Ghiselli G, Wang JC, Bhatia NN, et al. Adjacent segment degeneration in the lumbar spine. J Bone Joint Surg Am, 2004, 86-A(7): 1497-503.
4. Penta M, Sandhu A, Fraser RD. Magnetic resonance imaging assessment of disc degeneration 10 years after anterior lumbar interbody fusion. Spine, 1995, 20(6): 743-7.
5. Hoogendoorn RJ, Helder MN, Wuisman PI, et al. Adjacent segment degeneration: observations in a goat spinal fusion study. Spine, 2008, 33(12): 1337-43.
6. Park P, Garton HJ, Gala VC, et al. Adjacent segment disease after lumbar or lumbosacral fusion: review of the literature. Spine, 2004, 29(17): 1938-44.
7. Umehara S, Zindrick MR, Patwardhan AG, et al.The biomechanical effect of postoperative hypolordosis in instrumented lumbar fusion on instrumented and adjacent spinal segments. Spine, 2000, 25(13): 1617-24.
8. Akamaru T, Kawahara N, Tim Yoon S, et al. Adjacent segment motion after a simulated lumbar fusion in different sagittal alignments: a biomechanical analysis. Spine, 2003, 28(14): 1560-6.
9. Keorochana G, Taghavi CE, Lee KB, et al. Effect of sagittal alignment on kinematic changes and degree of disc degeneration in the lumbar spine: an analysis using positional MRI. Spine, 2011, 36(11): 893-8.
10. Aota Y, Kumano K, Hirabayashi S. Postfusion instability at the adjacent segments after rigid pedicle screw fixation for degenerative lumbar spinal disorders. J Spinal Disord, 1995, 8(6): 464-73.
11. Sears WR, Sergides IG, Kazemi N, et al. Incidence and prevalence of surgery at segments adjacent to a previous posterior lumbar arthrodesis. Spine J, 2011, 11(1): 11-20.
12. Cardoso MJ, Dmitriev AE, Helgeson M, et al. Does superior-segment facet violation or laminectomy destabilize the adjacent level in lumbar transpedicular fixation? An in vitro human cadaveric assessment. Spine, 2008, 33(26): 2868-73.
议题7:腰椎棘突间分离装置的临床应用:
----适应症到底在哪里?
本章节内容负责人:金大地教授 李淳德教授
腰椎棘突间分离装置(IPD) 设计的初衷是希望限制病变节段活动、撑开棘突间隙进而起到稳定腰椎节段及间接减压的作用【1,2】。尽管目前唯一得到美国FDA批准的X-Stop装置的使用指征仅为存在神经源性间歇性跛行的腰椎管狭窄症患者【3】,且近期的Meta分析指出由于较高的费用以及总体高达7%的严重并发症,目前尚不建议广泛推广棘突间分离装置【4】。尽管如此,随着各类装置的不断研发,有文献指出2007-2010年该类装置在世界范围内的使用量迅猛增加【5】;且在缺乏前期研究的基础上,其应用范围也被人为的不断扩大。而这在一定程度上也导致了该类装置并发症及翻修率的大幅上升【6,7】。基于上述事实,您认为:腰椎棘突间分离装置的临床适应症究竟是什么?
1. Tsai KJ, Murakami H, Lowery GL, Hutton WC. A biomechanical evaluation of an interspinous device (Coflex) used to stabilize the lumbar spine. J Surg Orthop Adv. 2006;15:167–172.
2. Wilke HJ, Drumm J, Haussler K, et al. Biomechanical effect of different lumbar interspinous implants on flexibility and intradiscal pressure. Eur Spine J, 2008, 17(8):1049-1056.
3. http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfTopic/pma/pma.cfm?nu...
4. Moojen WA, Arts MP, Bartels RH, et al. Effectiveness of interspinous implant surgery in patients with intermittent neurogenic claudication: a systematic review and meta-analysis. Eur Spine J, 2011. 20(10): 1596–1606.
5. ‘Sale numbers directly obtained from Kyphon Inc and Paradigm Spine Inc.’ from Moojen WA, Arts MP, Bartels RH, et al. Effectiveness of interspinous implant surgery in patients with intermittent neurogenic claudication: a systematic review and meta-analysis. Eur Spine J, 2011. 20(10): 1596–1606.
6. Kim DH, Shanti N, Tantorski ME, Shaw JD, Li L, Martha JF, Thomas AJ, Parazin SJ, Rencus TC, Kwon B.Association between degenerative spondylolisthesis and spinous process fracture after interspinous process spacer surgery.Spine J. 2012 Jun;12(6):466-472.
7. Tuschel A, Chavanne A, Eder C, et al. Implant survival analysis and failure modes of the x-stop interspinous distraction device. Spine,2011. Spine (Phila Pa 1976). 2013, 38(21):1826-31.
议题8:腰椎椎体间融合--微创 or 开放:
----优劣利弊的再审核!
本章节内容负责人:周跃教授 叶晓健教授
近年来,关于微创与传统开放腰椎椎体间融合术的临床对照研究逐渐增多【1-4】。虽然微创技术本身具有软组织损伤小、手术出血少、术后恢复快等诸多优势【3-4】。但目前仍有大量文献指出微创椎体间融合术具有更长的学习曲线、更高的并发症发生率、更多的放射线暴露等问题;同时部分综述性文献指出:微创椎体间融合术远期疗效并无明显优势【5-10】。且有学者认为脊柱微创领域被大量低质量的文献研究结果所“干扰”,甚至部分“公认”的微创技术优势都令人质疑,尚需要更多更为真实的数据来做出判断【11-12】。时至今日,我们是否有必要对微创椎体间融合术的优劣利弊进行再次审核?
1. Jaikumar S, Kim DH, Kam AC. History of minimally invasive spine surgery. Neurosurgery, 2002, 51(5 Suppl): S1-14.
2. Thongtrangan I, Le H, Park J, et al. Minimally invasive spinal surgery: a historical perspective. Neurosurg Focus, 2004, 16(1): E13.
3. Kim CW,et al. The Current State of Minimally Invasive Spine Surgery.J Bone Joint Surg Am. 2011;93:582-96.
4. Spetzger U, et al. The past, present and future of minimally invasive spine surgery: a review and speculative outlook. Minim Invasive Ther Allied Technol. 2013;22(4):227-41.
5. Arts M, et al. Does minimally invasive lumbar disc surgery result in less muscle injury than conventional surgery? A randomized controlled trial.Eur Spine J. 2011;20(1):51-7.
6. Fan SW, et al. Minimally Invasive Transforaminal Lumbar Interbody Fusion for the Treatment of Degenerative Lumbar Diseases. Spine 2010;35:1615–1620.
7. Fourney DR, et al. Does Minimal Access Tubular Assisted Spine Surgery Increase or Decrease Complications in Spinal Decompression or Fusion? Spine 2010;35:S57–S65.
8. CW Peng, WM Yue, SB Tan. Clinical Outcome of Minimally Invasive vs Open Transforaminal Lumbar Interbody Fusion. Spine 2009:34(13)1385-9.
9. Wang B, Lü G, Patel AA, et al. An evaluation of the learning curve for a complex surgical technique: the full endoscopic interlaminar approach for lumbar disc herniations. Spine J. 2011;11(2):122-30.
10. Wang J,Zhou Y,et al. Minimally invasive or open transforaminal lumbar interbody fusion as revision surgery for patients previously treated by open discectomy and decompression of the lumbar spine. Eur Spine J. 2011; 20(4):623-8.122–130.
11. Epstein NE. How often is minimally invasive minimally effective: what are the complication rates for minimally invasive surgery? Surgical Neurology. 2008; 70:386–389.
12. Schoenfeld AJ. Minimally Invasive Lumbar Fusion. Seminars in Spine Surgery. 2011;23(4):235-241.
议题9:腰椎融合术后融合器退移的原因分析:
----如何避免“你我之责”?
本章节内容负责人:罗卓荆教授 杨惠林教授
自1992年,第一例腰椎BAK椎间融合器临床应用至今已有22年的历史,期间腰椎椎间融合器在形态学、材料学以及临床操作技术等各方面均取得了巨大发展【1-4】。但退移问题始终伴随着融合器的整个发展过程【5-11】。融合器临床应用之初大多单独使用,随后的生物力学及临床研究表明单独使用缺少足够的力学稳定性,建议附加椎弓根螺钉固定【7-8】。但在椎弓根螺钉临床广泛使用之后,椎间融合器退移的临床发生率并未得到显著降低;且近年来多项临床研究提示融合器的退移与术中操作因素密切相关【8-12】。那么,对于该问题发生的具体原因究竟有哪些?我们临床医生该如何避免呢?
1. Bagby G. The Bagby and Kuslich (BAK) method of lumbar interbody fusion. Spine (Phila Pa 1976). 1999;24(17):1857.
2. Rauzzino MJ, Shaffrey CI, Nockels RP, et al. Anterior lumbar fusion with titanium threaded and mesh interbody cages. Neurosurg Focus. 1999;7(6):e7.
3. Spruit M, Falk RG, Beckmann L, et al. The in vitro stabilising effect of polyetheretherketone cages versus a titanium cage of similar design for anterior lumbar interbody fusion. Eur Spine J. 2005;14(8):752-8.
4. Cutler AR, Siddiqui S, Mohan AL, et al. Comparison of polyetheretherketone cages with femoral cortical bone allograft as a single-piece interbody spacer in transforaminal lumbar interbody fusion. J Neurosurg Spine. 2006;5(6):534-9.
5. Glassman SD, Johnson JR, Raque G, et al. Management of iatrogenic spinal stenosis complicating placement of a fusion cage. A case report. Spine (Phila Pa 1976). 1996;21(20):2383-6.
6. Elias WJ, Simmons NE, Kaptain GJ, et al. Complications of posterior lumbar interbody fusion when using a titanium threaded cage device. J Neurosurg. 2000;93(1 Suppl):45-52.
7. Oxland TR, Lund T. Biomechanics of stand-alone cages and cages in combination with posterior fixation: a literature review. Eur Spine J. 2000;9 Suppl 1:S95-101.
8. Uzi EA, Dabby D, Tolessa E, et al. Early retropulsion of titanium-threaded cages after posterior lumbar interbody fusion: a report of two cases. Spine (Phila Pa 1976), 2001, 26(9):1073-5.
9. Aoki Y, Yamagata M, Nakajima F, et al. Posterior migration of fusion cages in degenerative lumbar disease treated with transforaminal lumbar interbody fusion: a report of three patients. Spine (Phila Pa 1976), 2009, 34(1):E54-8.
10. Smith AJ, Arginteanu M, Moore F, et al. Increased incidence of cage migration and nonunion in instrumented transforaminal lumbar interbody fusion with bioabsorbable cages. J Neurosurg Spine, 2010, 13(3):388-93.
11. Kimura H, Shikata J, Odate S, et al. Risk factors for cage retropulsion after posterior lumbar interbody fusion: analysis of 1070 cases. Spine (Phila Pa 1976), 2012, 37(13):1164-9.
12. Abbushi A, Cabraja M, Thomale UW, et al. The influence of cage positioning and cage type on cage migration and fusion rates in patients with monosegmental posterior lumbar interbody fusion and posterior fixation. Eur Spine J, 2009, 18(11):1621-8.



 京公网安备11010502051256号
京公网安备11010502051256号